What are Social Determinants of Health?
Social determinants of health (SDOH) is a term used to describe the conditions where people live, learn, work, play, and age that directly affect their health outcomes and risks. While the ability to influence these factors has traditionally been viewed as something outside the role of clinical care, government initiatives are placing increasing responsibility for a patient’s whole health on their provider, making it essential for healthcare organizations to identify and address SDOH.
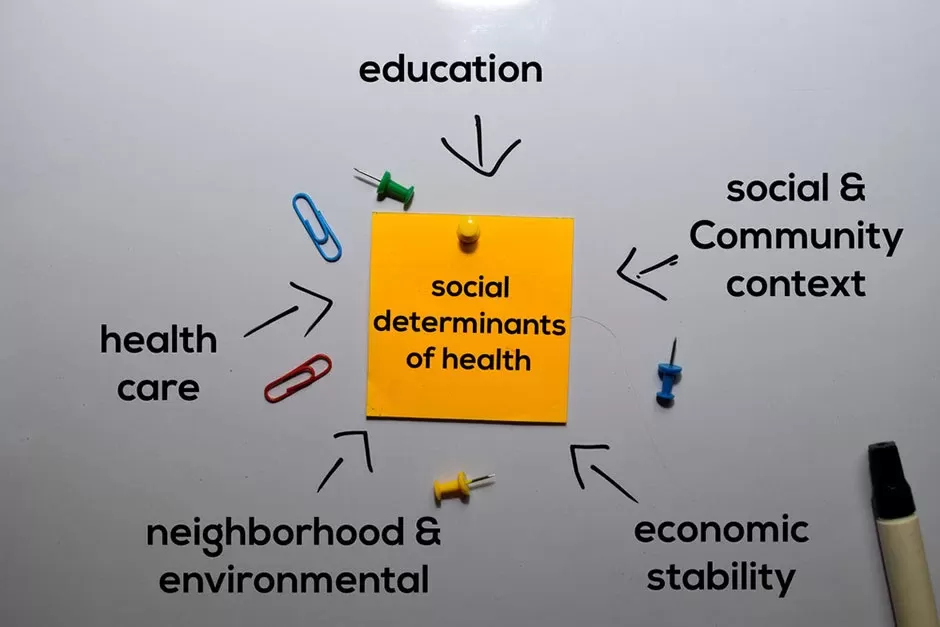
Examples of Social Determinants of Health
There are many conditions classified as SDOH, and these factors are often grouped into five broad categories: Economic stability, education, social and community context, health and healthcare, and neighborhood and built environment. The following are specific examples of conditions from each category:Economic Stability
- Socioeconomic conditions, such as income level
- Job opportunities and access to job training
- Food Insecurity
- Housing Instability
Education
- Access to education and the quality of available education
- Early childhood experiences and development
- Literacy levels
Social and Community Context
- Social norms and attitudes
- Discrimination
- Incarceration
Health and Healthcare
- Access to health care services
- Health literacy levels
Neighborhood and Built Environment
- Living conditions such as housing status
- Access to clean water and healthy foods
- Exposure to crime, violence, and social disorder
- Access to public transportation
The Impact of Social Determinants of Health
To underscore the importance of SDOH, consider this: According to the U.S. Centers for Medicare and Medicaid Services, domestic health care spending increased 4.6 percent in 2018, reaching $3.6 trillion or $11,172 per person. However, despite more resources being spent on health care services, overall health outcomes are not increasing in turn. Surveys have shown the average life expectancy in the U.S. has been declining for several years, and death rates due to cardiometabolic diseases such as heart disease, stroke, and diabetes have held steady or increased since 2010, according to research in JAMA. “It is shocking that the United States, with its vast resources, continues to see increases in preventable deaths,” said Jennifer Frost, M.D., tells the American Academy of Family Physicians. While many factors influence these trends, data has shown medical care actually has a much smaller impact on overall health outcomes than SDOH. In fact, Aligning for Health estimates that SDOH represent 80 to 90% of the modifiable factors that influence health outcomes, while medical care only accounts for 10 to 20%.How Healthcare Organizations Can Address SDOH
Given the large impact of SDOH on health outcomes, it is crucial for healthcare organizations to remain cognizant of SDOH and find ways to address these factors when providing care to patients. “It is critical to be aware that addressing health-related social needs of patients is essential to achieving goals of high quality and high-value care,” Kirsten Bibbins-Domingo, PhD, MD, MAS, professor and chair of the Department of Epidemiology and Biostatistics at the UCSF School of Medicine, explained to HealthLeaders. There are a number of initiatives and guidelines aimed toward helping healthcare organizations address SDOH, including resources from the U.S. Centers for Disease Control and Prevention and the National Academies of Sciences, Engineering, and Medicine. Many of these tools recommend the following steps for healthcare providers.- Implement Social Screening To better address SDOH, healthcare organizations may want to consider using social risk screening questions to achieve a more comprehensive understanding of their patient’s needs. A recent study published in JAMA found only 24% of hospitals and 16% of physician practices currently screen for these factors.
- Adjust Clinical Care to Address SDOH When healthcare providers are aware of their patients’ social needs, they are better able to make adjustments to provide better, more effective care. Some examples might include providing simplified care instructions for patients with low health literacy or offering telehealth services to those who struggle to visit the facility due to lack of access to public transportation.
- Connect Patients with Appropriate Resources With a better understanding of patients’ social situation, healthcare providers can help educate them about eligibility for and access to programs such as Medicaid, SNAP, or TANF.
Guideway’s Care Guidance services identify and address the barriers and issues hidden within social determinants of health.
Fill out the form below to learn how Guideway Care addresses social determinants in order to improve outcomes and satisfaction and lower the cost of care.Contact Us Today To Learn How We Can Help
"*" indicates required fields