Patient Satisfaction in Healthcare: What It Is, Why It Matters & How to Improve It
Patient satisfaction: a subjective measure of whether a patient’s expectations about a health encounter were met.
Patient satisfaction can be a loaded term. Patients want a great care experience, and the focus of physicians and nurses is to provide great health care, but these two priorities are not always aligned. Patient satisfaction doesn’t always correlate with the best outcomes. Furthermore, resource constraints and organizational dysfunction can prevent clinical staff from providing the type of care experience that both they and their patients desire. These tensions, along with increasingly profound financial implications for hospitals providing care, factor into the debate about how to objectively describe patient satisfaction, the best ways to measure it, and how to ethically and effectively incentivize hospitals and providers to improve it.
History of Patient Satisfaction
Despite its current importance, the concept of “patient satisfaction” hasn’t always been around. The Press Ganey company was started in 1985 by two Notre Dame professors, Irwin Press and Rod Ganey. Press (a medical anthropologist) and Ganey (a sociologist and statistician) created a new market by applying reliable survey design and administration to healthcare. As Press Ganey’s influence grew, hospitals began to realize the importance of being able to quantify, track and compare their patients’ levels of satisfaction with the care they received. Demand continued to increase for these types of survey services, and additional firms such as Gallup, NRC, PRC, HealthStream, and Avatar entered the market. As the use of patient surveys spread throughout hospital departments, survey companies began to offer advice on how to improve patient satisfaction. Eventually, the interest in and efforts towards improving patient satisfaction caught the attention of the federal government and led to the first federally-backed survey of patient satisfaction, called HCAHPS.HCAHPS
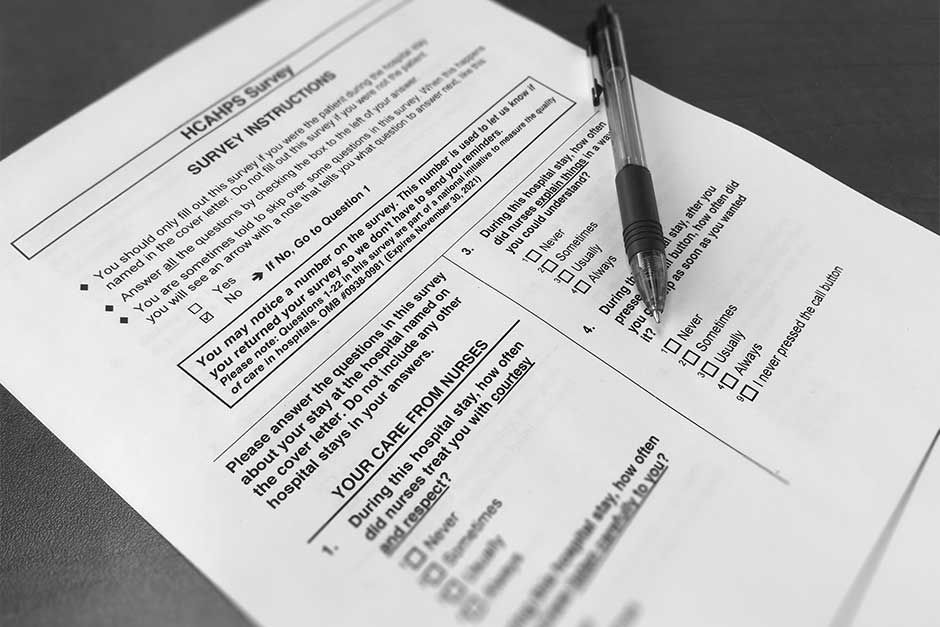
In 2002, the Centers for Medicare and Medicaid Services (CMS) and the Agency for Healthcare Research and Quality (AHRQ) worked together to research, develop, and test the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey – the first national, standardized, publicly-reported survey of patients’ perspectives of hospital care. The implementation of HCAHPS began in October of 2006, with the first public HCAHPS score reports issued in March 2008. HCAHPS is a standardized survey administered by approved vendors or the hospital. The survey is randomly provided to adult hospital inpatients between 48 hours and 6 weeks after discharge. The HCAHPS survey contains 21 patient perspectives on care and patient rating items that encompass nine key topics:- Communication with doctors
- Communication with nurses
- Responsiveness of hospital staff
- Pain management
- Communication about medicines
- Discharge information
- Cleanliness of the hospital environment
- Quietness of the hospital environment
- Transitions of care
Patient Satisfaction vs. Patient Experience
The terms “patient satisfaction” and “patient experience” mean two different things, even though they are often used interchangeably. According to the Agency for Healthcare Research and Quality (AHRQ): “To assess patient experience, one must find out from patients whether something that should happen in a health care setting (such as clear communication with a provider) actually happened or how often it happened. Satisfaction, on the other hand, is about whether a patient’s expectations about a health encounter were met. Two people who receive the exact same care, but who have different expectations for how that care is supposed to be delivered, can give different satisfaction ratings because of their different expectations.” In reality, many “patient satisfaction” surveys are actually trying to objectively determine whether the necessary processes are in place for an optimal patient experience. In fact, HCAHPS asks “‘how often’ or whether patients experienced a critical aspect of hospital care, rather than whether they were ‘satisfied’ with their care.” The terms are closely related, however, and if a hospital can improve the concrete details of patient experience, they have a better chance of improving in the much more subjective area of patient satisfaction.Why It Matters
Patient Experience and Outcomes
Patient experience is a quality area measured under the 2016 CMS Hospital Value-Based Purchasing (VBP) Program. Patient experience accounts for 25 percent of a hospital’s VBP score. In addition, patient experience is one of the three tenets of the “Triple Aim” of healthcare:- Improving the patient experience of care
- Improving the health of populations
- Reducing the per capita cost of healthcare
Financial Implications for Hospitals
Hospitals and providers are increasingly bearing the brunt of the federal government’s drive to link reimbursements to patient experience scores. Under VBP, a percentage of Medicare reimbursements (currently 2%) is withheld. Withholdings are redistributed to hospitals based on their Total Performance Scores (TPS) that they earn for the year. A hospital could earn an amount less than, equal to, or more than the amount originally withheld. TPS scores are based on their performance on quality and resource use measures. Patient experience is one of four domains scored under VBP, which include four equally-weighted categories:- Clinical Care
- Patient Experience of Care/Person and Community Engagement (scores taken from HCAHPS survey)
- Safety
- Efficiency and Cost Reduction
How to Improve Patient Satisfaction
Having the processes in place for an optimal patient experience paves the way for higher patient satisfaction ratings. Advice varies on improving patient experience, but can be boiled down to the following:- Improve care coordination
- Ensure adequate nurse staffing
- Train doctors and nurses in more effective communication strategies
More Patient Satisfaction Resources:
- How Can Nurses Improve Patient Satisfaction?
- Improving Patient Satisfaction: 5 Low-Cost Strategies
- Improve Patient Satisfaction With Care Guidance
Take the first step to improving patient satisfaction at your hospital. Contact for more information about Guideway’s care guidance program today.




